The Telegraph
The midlife health checks you should never skip – and the ones worth paying for
Lebby Eyres – November 21, 2022
We’ve all heard the expression “Life begins at 40” – but, unfortunately, 40 is also the age when life starts to catch up with us. The gloomy truth is that if you’re drinking, smoking, eating a bad diet and sitting on your sofa a bit too much, you’re four times more likely to die in the next decade than your smoothie-drinking, teetotal, marathon-running mate.
But help is at hand, because even if those party invitations are petering out, midlife is when the NHS screening invites start to arrive. Even if you feel on top of your game and are symptom-free, it’s best not to ignore them – especially as it’s estimated around three million people missed screening appointments when most services were paused at the beginning of the pandemic, contributing to the 39,000 missed cancer diagnoses from April 2020 to March 2021. As a result, more people will be diagnosed at a later stage, meaning their cancer may be harder to treat or even incurable.
Despite this, around 30 per cent of us don’t go to the tests we’re entitled to. According to recent NHS figures, only 70 per cent of cervical cancer screening invitations were accepted, while mammograms were taken up by 64 per cent and only 71 per cent responded to bowel cancer screening invitations in 2022.
Preventative screening of a healthy population is different from diagnostic testing when symptoms are present. Dr James Gill, clinical lecturer in clinical skills at Warwick University, explains, “A test would be, ‘We think this is going on – can we find it?’ With screening, we are saying, ‘We don’t think anything is going on – but can we see any evidence of something going on early?’ Effective screening has three crucial features: to be able to identify a disease early on, to have a reliable test and, as a result of the first two, you must then be able to affect the course of disease to result in a positive outcome.”
In Britain, the independent UK National Screening Committee makes recommendations about screening programmes to ministers based on evidence, benefit vs harm ratio and cost-effectiveness.
You might ask why we don’t screen everyone in the relevant age bracket, every year for all the key cancers. Dr Samar Mahmood, a GP and clinical lecturer from South Yorkshire, explains: “So, more screening equals more cancers diagnosed, yes. But also more false positives and more harm to the additional people who ended up having further unnecessary tests [such as scans or biopsies]. There is a sweet spot, and the NSC crunch the numbers on this.”
Our national screening programmes are similar to other countries. Most focus on breast, bowel and cervical with some variation in frequency and age screening starts. Mammograms are offered every two years in France and Ireland from 50. Germany offers men aged 50 and women aged 55 a colonoscopy once every nine years, and a skin cancer check every two years to over-35s. In America, cervical screening begins at 21, and in Australia women can ask for a mammogram from 40 every two years.
But what is the situation in the UK? Here are the essential screening tests you’ll be invited to on the NHS.
The screening: the NHS Health Check
When you have it on the NHS: From aged 40, and repeated every five years
How you get it: In theory, you should be invited as everyone is entitled to a test but funding was paused during the pandemic. Dr Mahmood urges the over-40s to, “Check with your GP surgery whether or not you will be invited.”
If you encounter a problem, check with your local authority as they are also available in pharmacies and mobile units.
What’s involved: Dr Mahmood says, “It’s a five-yearly MOT that consists of a set of routine blood tests and measurements of height, weight, blood pressure. It can pick up on signs you might develop certain diseases in the future, including diabetes and high blood pressure, whether you have anaemia, how high your cholesterol is, or, if you are clinically overweight.”
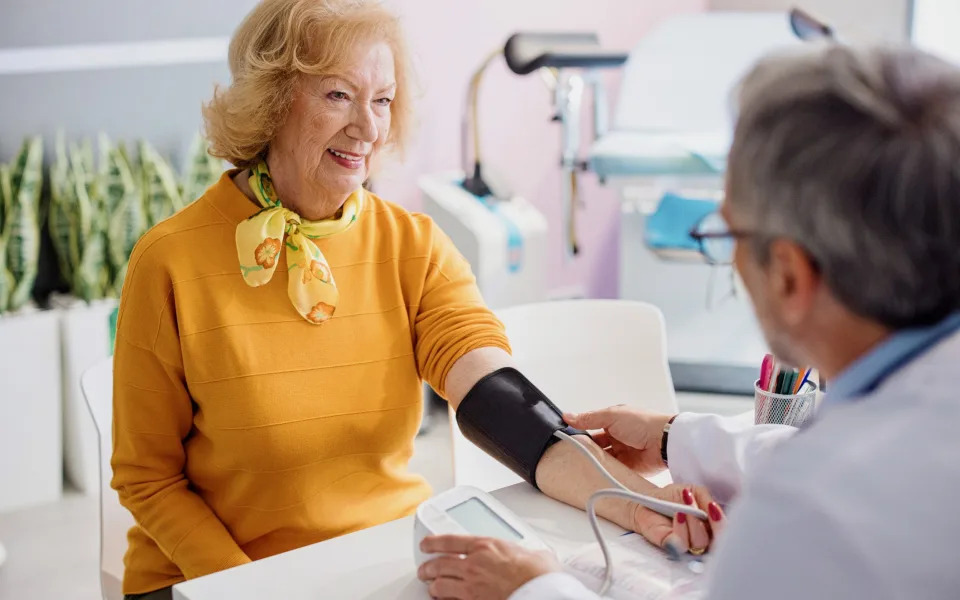
Why it’s important: High BP (over 140/90) is a risk factor for kidney and heart disease and stroke and an indicator of diabetes. Your GP or nurse will calculate your “QRISK” score for cardiovascular disease using your results, which is the likelihood of having a heart attack or stroke in the next ten years.
What if you have an abnormal result?
“Any abnormalities picked up on the blood tests will then be reviewed further by the GP,” says Dr Mahmood. The GP may carry out a HbA1c test to see if you have diabetes. A QRISK score of over 10 per cent could result in statins being prescribed, while heavy drinkers could be offered a liver scan. Finally, the test may pick up if you have an increased risk of dementia. Lifestyle changes may be advised.
The screening test: Breast cancer screening
When you have it on the NHS: every three years from age 50-71 or annually from 40 for high-risk women.
How you get it: you should be sent an invitation by your GP, breast screening unit or hospital (if high risk). You must be registered with a GP.
Why it’s important: Eight out of ten breast cancers occur in women over 50. “We’re trying to find evidence for the disease early on before it becomes noticeable,” says Dr Gill, “and we’re trying to prevent a greater level of disease burden by treating these patients early.”
What’s involved: A mammographer will take two X-rays of each breast. It can be slightly uncomfortable but is a very quick procedure.
What if you have an abnormal result?
You’ll receive a letter with results, and diagnostic tests may take place such as another mammogram, ultrasound and biopsy.
The screening test: Cervical cancer screening
When you have it on the NHS: Women aged 25 to 49 have it every three years, and from 50 to 64 it changes to every five years.
Why it’s important: Around 3,200 cases are diagnosed each year. Fifty per cent survive for 10 years or more. “The vast majority of cervical cancers are due to HPV, Human Papilloma Virus,” says Dr Gill. “But even if someone isn’t sexually active, or has never had sex with men, it’s still advisable to have a cervical cancer screening, because not all causes are due to an HPV.”

What’s involved: A smear test. Although the process is the same, there is now a new test which screens for the HPV virus first. If it is positive, your sample will be tested again to see if there are changes in the cells.
What if you have an abnormal result?
“If you’re positive for signs of HPV, we’ll make sure you are called in more frequently,” says Dr Gill. This is usually annually. If you are positive for HPV and have abnormal cells, you’ll have a colposcopy.
The screening test: Bowel cancer screening
When you have it on the NHS: Every two years for people aged 60-74 – although this is gradually being lowered to age 50.
How you get it: You’ll be sent a faecal immunochemical test in the post, which you send back. “It’s the most minimally invasive screening test you could have and looks for evidence of blood in the stool,” says Dr Gill. “A haemoglobin level of below 120 in women and 130 in men is an indication for a possible bowel cancer – patients will be sent a FIT test.”
Why it’s important: There are 16,800 cancer deaths in the UK every year, and it’s the second biggest cancer killer, yet 98 per cent will survive for a year or more if treated in the earliest stages.
What if you have an abnormal result?
Around 2 per cent of FIT tests are abnormal and patients are normally referred for a colonoscopy.
The screening test: Aortic Abdominal Aneurysm
This is for a swelling of the main blood vessel that leads from the heart to the abdomen.
When you have it on the NHS: Men aged 65 are offered a one-off screen.
How you get it: You should be invited by your GP but if you are 65 and have not received one then contact your local screening service.
Why it’s important: “If you have an AAA and it leaks or bursts in the community, your chance of dying is 90 per cent,” says Dr Gill.
What if you have an abnormal result?
“Sometimes we’ll keep an eye on it until it’s grown big enough that the risks of surgery outweigh the risks of leaving it,” says Dr Gill. “Once it’s big enough, we will go in to try and essentially line it with Gore-Tex to stop it bursting.”
The test: Prostate specific antigen test
When you have it on the NHS: There is no prostate screening on the NHS, as the benefit may not outweigh the harm. “The PSA test is not reliable,” says Dr Gill. “Sexual activity, vigorous exercise and eating a large amount of meat can throw off the PSA test, which is why we do it in a controlled situation.”
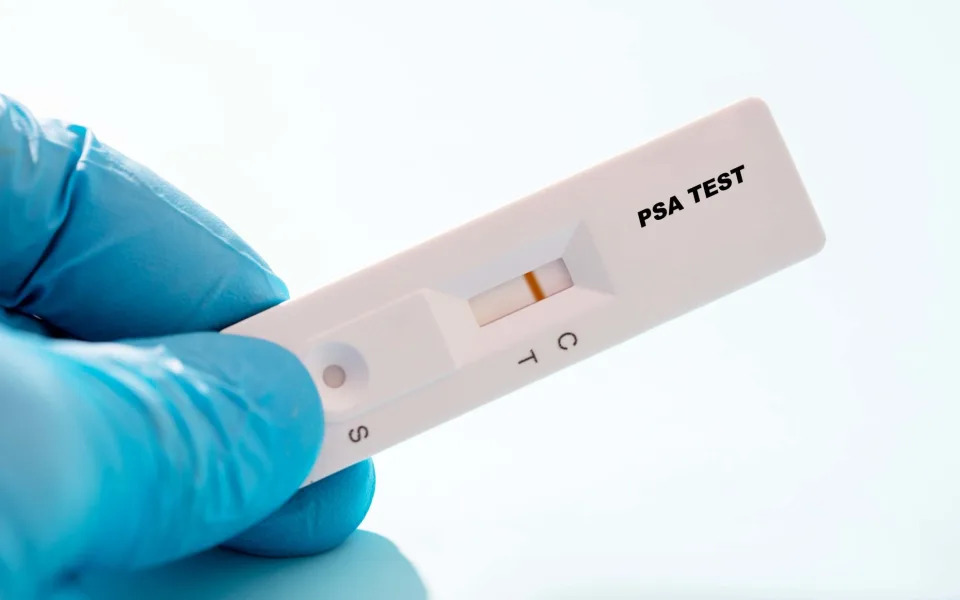
How you get it: Healthy men over 50 can ask for a PSA test via the NHS informed choice programme.
Why it’s important: In 2018, Prostate cancer became the third biggest cancer killer in the UK. in February, Prostate Cancer UK launched a Find the 14,000 Men campaign with the NHS to urge men to check their risk online and talk to their GP if they are: prostate cancer accounts for over a third of undiagnosed cancers during the pandemic.
What if you have an abnormal result?
PSA testing has a high number of false positives, and one in seven are false negatives. A positive result may result in further investigation including an MRI, sometimes followed by a biopsy. “Prostate biopsies can cause infections, impotence and bowel issues,” says Dr Gill.
Finally, although it has not been rolled out yet, in June this year, the UK NSC recommended the first national lung cancer screening programme, targeted at people aged 55-74 at high risk. When it is rolled out, people who smoke or used to smoke may be offered a low-dose CT scan.
Private healthcare providers also offer all of the above screening at your own convenience and in comfortable surroundings. Healthcare charity Nuffield Health provides 360 health assessments which offer additional non-invasive tests. Dr Kim Goldin, Senior General Practitioner and Clinical Lead for Nuffield Health’s GP team, says, “NHS Health Check is a very good baseline but there is more you can add on. For example, at Nuffield, we offer a HbA1c test, urate test and, for women over 50, TSH levels, Which test respectively for diabetes, gout and also metabolic diseases, and thyroid issues.”
But is it worth screening for cancer, or other illnesses, more often than the NHS advises? Not according to Dr Mahmood. “While there may be no long-lasting damage from a one-off private CT scan or X-ray, if somebody was frequently getting it done as part of a private screening test then there could be a chance of radiation-related cancer in itself,” he says. “The other thing to consider is harm in other ways. For example, regular private screening might indicate that somebody has health anxiety and perhaps the answer to this is to speak to their GP rather than get a screening test done.”
If you have symptoms, however, that could be a different matter.
The tests worth paying for

In October, it was revealed that in August, 461,400 people had been waiting six weeks or more for one of 15 key diagnostic tests including an MRI or ultrasound. Some patients are choosing to go private, but how do you do that and what should you be aware of? Dr Mahmood answers the key questions.
Q: I’m worried about waiting. How do I get a diagnostic test done privately?
A: You can approach any private healthcare provider and ask whether they carry out the test you are interested in. For simple tests, such as blood tests or ECG, a consultation with a doctor is not required beforehand. For something more invasive, such as an endoscopy, you may need to consult with a clinician before they are able to recommend the test for you.
Q: Can I self-refer?
A: For a private consultation with a doctor, most providers will want a referral letter from your NHS GP. However, for the private tests (without a specialist consultation) mentioned above, a self-referral will usually be accepted.
Q: Can a GP access private health diagnostic results and vice versa?
A: GPs do not have access to private diagnostic results, other than paper copies of your results which you would need to provide them with. Similarly, private providers cannot access your NHS results/health records unless you provide them.
Q: What happens if I have an abnormal result?
A: Ordinarily, unless your private test is done following a private consultation with a specialist who will follow your case up, you would go back to your NHS GP for further management. Be aware it can be hard for the GP to interpret another provider’s test result without the context behind why the test was done.
